What does polyneuropathy mean?
The word polyneuropathy is basically composed of the words poly = many, neuro = nerves and pathie = disease. Polyneuropathy is thus translated as the disease of many nerves.
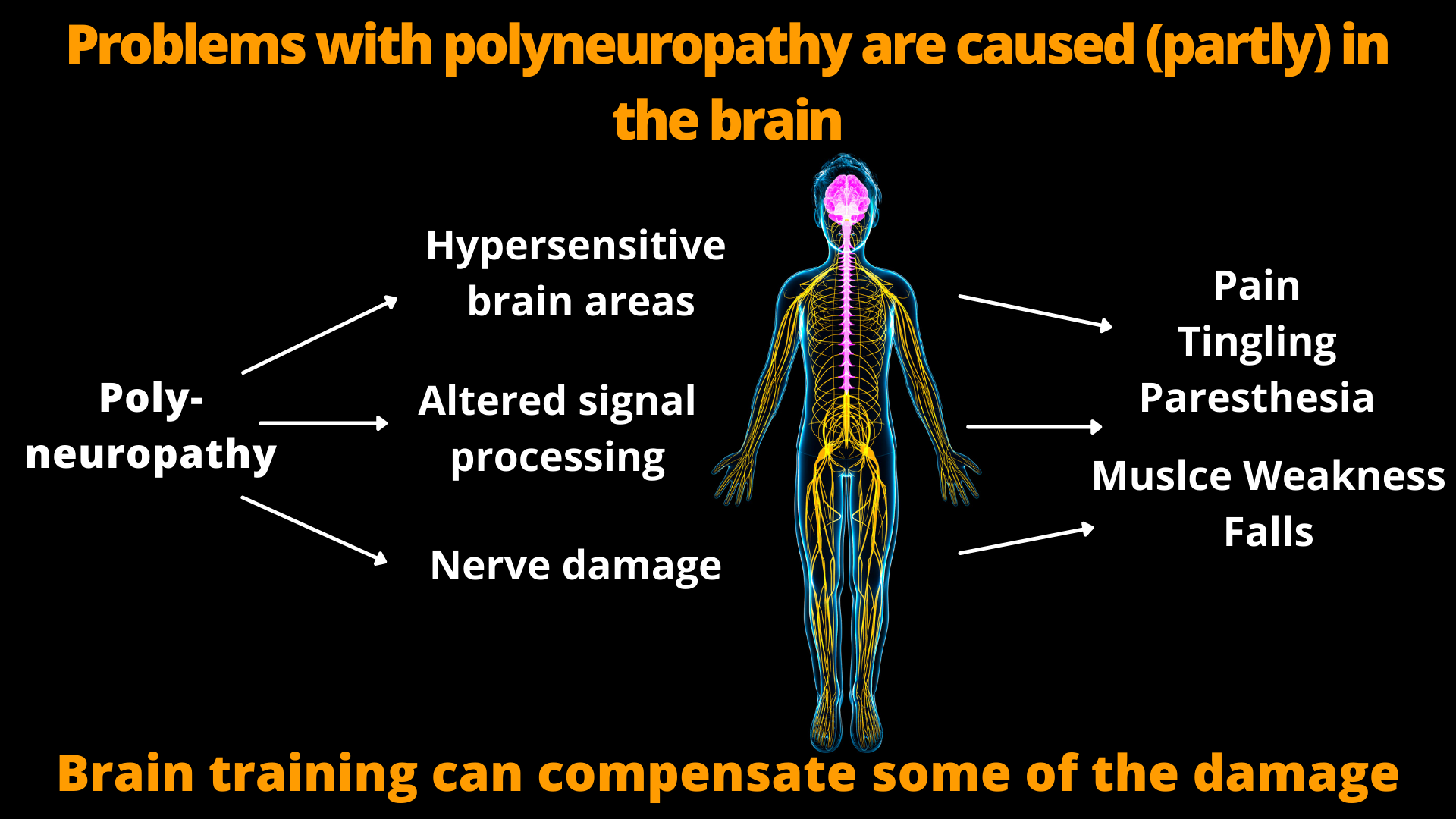
In our body there are countless nerves, which you can think of as cables for signal transmission. They bring signals from our body to the brain. These are perceived and processed there. Your brain processes these signals to feelings of touch, movement or pain.
In addition, the nerves bring signals from the brain and spinal cord to the muscles and organs. This allows the brain to send commands to the rest of the body.
Polyneuropathy disrupts this signal transmission. Therefore, disturbances in body perception, i.e. numbness, tingling, pain and other unpleasent sensations may occur. Approximately 50% of patients report such discomfort or pain; the other half merely lose all sensation to the affected body part without developing discomfort or pain.
In addition, loss of muscle strength and even paralysis can occur because signals from the brain no longer reach the muscles. The same might happen with other organs.
How exactly polyneuropathy manifests itself, i.e. whether one has pain or loses muscle strength, and also how severe the disease becomes and how quickly it progresses depends on many different factors. For example, there are numerous people who simply have no feeling in their feet because of polyneuropathy, but do not develop pain. Often they don't even feel it if they suffer an injury to their feet. On the other hand, there are people for whom even the slightest touch triggers incredible pain. How exactly polyneuropathy manifests itself therefore varies greatly between individual patients.
(For more information on pain in polyneuropathy, click here: Pain in Polyneuropathy and what you can do about it.
What are the different types of polyneuropathy?
Of course, there are many different forms this nerve diseases and, therefore there is basically not just one polyneuropathy. There are several factors according to which polyneuropathy is classified.
The simplest distinction is between sensory and motor polyneuropathies. Sensory polyneuropathy changes how you perceive your body because the nerves that are responsible for sensing it are damaged. This results in either numbness or pain and discomfort. In motor polyneuropathy, the nerves that carry signals to the muscles are damaged. As a result, you lose muscle strength, which can lead to the point where certain muscles can no longer be activated at all. Very often, however, damage to motor and sensory nerves occurs simultaneously.
In addition, polyneuropathies are classified according to which structures are damaged first. The nerve cell (neuron) itself, or the nerve processes (axons) and their myelin sheath can be affected.
What are the causes of polyneuropathy?
There are numerous, very different causes of polyneuropathy. In total, up to 500 different causes are known. In some forms, the nerves are directly affected. This is especially the case with infections and overreactions of the immune system (autoimmune diseases).
Infectious diseases that can cause polyneuropathy include Lyme disease, HIV, and hepatitis B and C.
In addition, the patient's own immune system may attack the nerves. In most cases, the myelin layers of the nerves are attacked. These form a sheath around the nerve endings that helps with signal transmission and supplies the nerves with nutrients. When it is destroyed, the nerves are massively affected. This is the case in chronic inflammatory demyelinating polyneuropathy and Guillain-Barré syndrome. Chronic demyelinating polyneuropathy, unlike most other polyneuropathies, progresses in flare ups. That is, the condition is relatively stable for a long time and suddenly deteriorates.
Guillain-Barré syndrome, on the other hand, occurs suddenly and progresses very quickly. It can lead to severe symptoms within a few days, although they often resolve completely.
Disturbances in blood circulation and metabolism can also trigger polyneuropathy. This is especially often the case in diabetics. In addition, a lack of oxygen can lead to polynueropathy; this can occur, for example, in sleep apnea.
Deficiency of certain vitamins (vitamin D and B vitamins) can also cause polyneuropathy. This can occur not only when you take too few vitamins with food. So-called malabsorption disorders, in which some nutrients cannot be absorbed properly, can also cause vitamin deficiency and subsequently polyneuropathy. The same applies to large alcohol consumption, which can lead in particular to a deficiency of vitamin B1, which in turn can lead to nerve damage and polyneuropathy.
Polyneuropathy due to poisoning
In addition, the nerves can be damaged by poisoning, which can also lead to polyneuropathy.
Polyneuropathies are often caused by poisoning with the following substances:
- Alcohol
- Lead and other heavy metals
- Solvent
- Pesticides
- Medications: chemotherapy, statins (cholesterol-lowering drugs if taken for a long time and in high doses).
Some drugs are thought to be able to cause polyneuropathies through drug interactions(Löscher et al 2017)
This list is not complete, there are numerous substances and drugs that are suspected of causing polyneuropathies, but for which this has not yet been conclusively clarified.
Polyneuropathy as a consequence of other diseases
In very many cases, however, polyneuropathy develops as a consequence of other diseases. These are for example:
- Diabetes
- chronic kidney failure
- Thyroid Diseases
- Liver disease
- Disturbances in the absorption of nutrients (malabsorption disorders)
- Sleep apnea
Often different causes add up
So as you see that there are countless forms and causes of polyneuropathy. As many as 500 different causes of polyneuropathy are described in the literature.
However, in about 35% of the cases it is not possible to find a cause at all.
In addition, there are people who have diabetes or are alcoholics and yet their nerves remain healthy, while others develop polyneuropathy even though they have none of these problems.
I therefore assume that it is often a multifactorial disease. This means that the development of polyneuropathy is an interaction of different things and cannot be attributed to a single cause in many people.
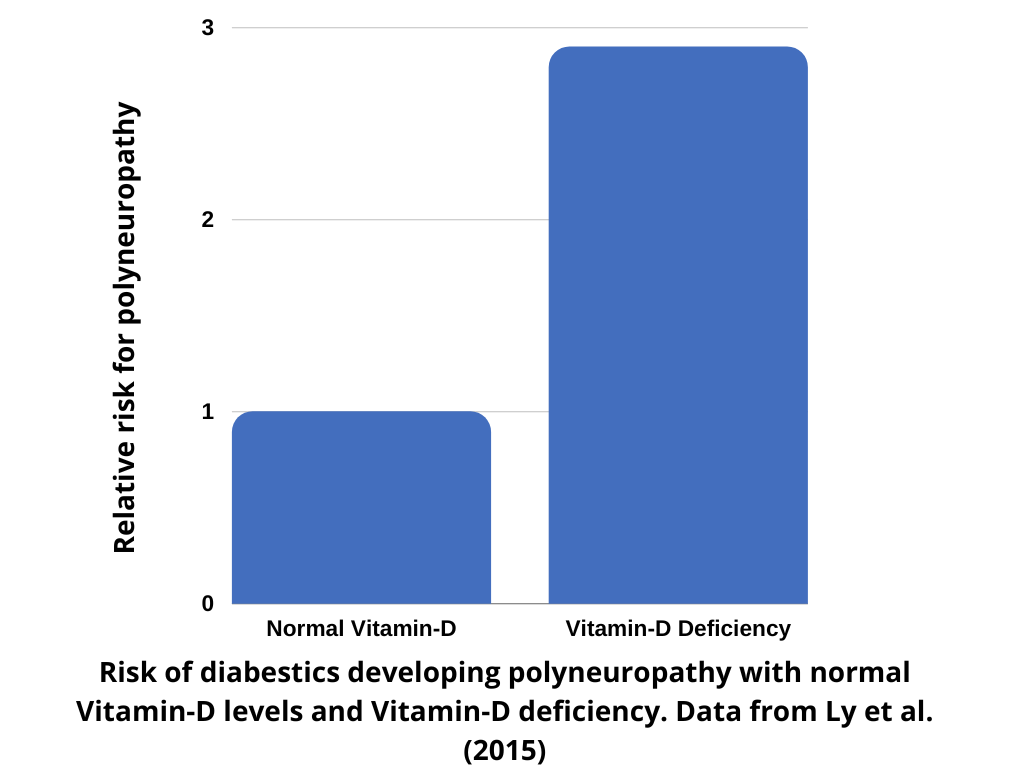
For example, the risk of developing polyneuropathy in diabetics is much lower if they have healthy levels of vitamin D in their blood(Qu et al. 2017). Other nutrients such as B vitamins may also play a role. So when diabetes and vitamin deficiency come together, polyneuropathy is more likely to occur. If, in addition, a lot of alcohol is consumed, another factor comes into play. Which of these factors then is the exact cause is basically impossible to diagnose.
You can find more about nutrition in polyneuropathy here: Nutrition in polyneuropathy, Vitamin D and polyneuropathy. (In German)
One protective factor for your nerves is good blood perfusion. Therefore, physical fitness can provide some protection. Because those who are physically fit also have better functioning blood vessels. However, if you are simply unlucky and have a genetic predisposition to polyneuropathy, then even if you have perfect nutrition and blood circulation, you can still develop polyneuropathy.
You can see that many factors affect polyneuropathy and the disease is very complex. Therefore, there is no "the" specific drug for polyneuropathy.
Nutrition in polyneuropathy
In polyneuropathy, certain forms of nutrition can be helpful and others can be harmful. In particular, there should be no deficiency of vitamins and nutrients. Therefore, extreme diets such as vegan, gluten-free or diets that are extremely low in salt should be avoided unless there is a medical reason for them. Such diets bring the risk of nutrient and vitamin deficiencies that can exacerbate polyneuropathy.
On the other hand, there are a few supplements, such as omega-3 fatty acids, that may be helpful in some forms of polyneuropathy.
You can find a detailed article about this here: Nutrition in polyneuropathy
Is there really no treatment for polyneuropathy?
Although it is said very often, it is not true that there is no treatment for polyneuropathy
Let's take of a person with diabetes, vitamin deficiency and high alcohol consumption for example. Let's assume this person receives medication for diabetes, exercises more and eats less sugar. This will improve the diabetes. The person also receives vitamin supplements to correct the deficiency and gives up drinking. The polyneuropathy would definitely develop better than if no measures were taken. The polyneuropathy was thus at least slowed down in its progression, even if there is no complete cure.
Thus, treatment of polyneuropathy is certainly possible. However, the disease is so complex that there is no single treatment that is sufficient on its own. If you take the right measures such as proper physical training, proper nutrition and medical treatment, you can usually at least slow down the progression of the disease or compensate for the limitations to some extent. However, treatment options differ from case to case and from person to person.
You can find more on this topic here:
Exhaustion and fatigue in polyneuropathy
Chronic fatigue is a common problem in polyneuropathy. Many patients do not know that exhaustion and fatigue are related to the disease. There are five factors that scientific studies have identified as causes of fatigue:
- Sleep problems due to pain and discomfort
- Overloaded muscles due to the changes in movement patterns in polyneuropathy.
- Reduced physical activity
- Depressed mood
- Side effects of medication
If these causes of exhaustion are known, they can often be treated and improved. This can often reduce fatigue.
How is polyneuropathy diagnosed? The diagnosis
To determine polyneuropathy, doctors usually first perform an examination of the reflexes. This is done by tapping the tendon at the front of the knee (patellar tendon) and the Achilles tendon with a reflex hammer. In response, the muscle twitches. If this does not work, this is an indication that a disturbance of the nerves and a polyneuropathy could be present.
Sensory tests are also carried out. For example, it is examined whether the patient can the vibration of a tuning fork. The sensation of warmth and cold is also investigated by touching warm or cold objects.
It is also very important where the patient feels discomfort or loss of sensation. Typically, symptoms first appear on the tips of the toes or fingers. This is because the path from the tips of the toes or fingers to the brain is the longest path. The nerves that present them therefore present the biggest area for damages to accumulate in. If the symptoms appear in other places or, for example, only in one foot or hand, the physician can draw conclusions about the type of polyneuropathy.
The type of the symptoms also already suggests which nerves are affected. When myelinated fibers are affected, limitations in the sense of touch, vibration, and body position, as well as decreased reflexes are more likely. When the unmyelinated fibers are affected, disturbances in pain and temperature sensation are present more often. In most cases, however, both types of nerves, myelinated and unmyelinated, are affected.
However, to diagnose polyneuropathy with certainty, it is usually necessary to examine the conductivity of the nerves. Thus, an electrical impulse is passed through the nerves. In patients with polyneuropathy, impulses are transmitted more slowly. In addition, in polyneuropathy, the electrical impulse (the amplitude) changes.
The examination of nerve conduction velocity also makes it possible to determine precisely which fiber types are damaged at which locations and to what extent. Thus, very precise statements can be made about the nerve damage.
However, there are also polyneuropathies in which the conductivity of the nerves remains normal. This is particularly the case in small-fiber polyneuropathy. This can be determined, for example, by skin biopsies.
How often does polyneuropathy occur?
Very many patients feel alone with polyneuropathy. Very few friends and acquaintances know what polyneuropathy is, and from the medical personnel you usually only hear that there is nothing they can do for you.
It might make you feel better to learn that the polyneuropathy is way more common than you think. Among those over 60, 7% are affected (Hanewinckel et al. 2016). In Germany, therefore, almost one million people suffer from this disease and we must assume that the number of unreported cases is considerable.
So polyneuropathy is a common disease, which nevertheless receives little public interest. In the following paragraphs will describe how often certain forms of polyneuropathy occur. The data come from a study by a research group led by Rens Hanewinckel of the University of Rotterdam (Netherlands) They combined data from numerous other studies to provide an overview of the data. The original scientific article from the European Journal of Epidemiology can be found here: Hanewinckel et al. 2016.
Polyneuropathy affects women and the elderly more often
The risk of developing polyneuropathy increases with age. On the one hand, this is due to the fact that in old age one is more susceptible and less capable of regeneration. In addition, at an older age, people are more likely to suffer from diseases that can result in polyneuropathy, such as cancer, diabetes, or kidney disease.
In addition, women suffer from polyneuropathy more often than men. Statistically, there are 1.5 women with polyneuropathy for every man with polyneuropathy. However, the reason for this has not yet been clarified.
Alcoholics are affected much more often
The exact number of alcoholics with polyneuropathy is not known. However, it is known that the risk of developing polyneuropathy is about four times higher in alcoholics than in the general population. By the way, alcohol can damage the nerves in several ways: It affects the nerves directly through the toxic effects of alcohol, and it also deprives the body of B vitamins, the deficiency of which can also trigger polyneuropathy. Here, the damage from vitamin deficiency seems to affect larger nerve fibers more, leading to motor deficits, whereas the direct toxic effect of alcohol seems to affect small sensory nerves more.
How common is polyneuropathy in diabetes?
Diabetes can lead to nerve damage and therefore cause polyneuropathy. The number of people with polyneuropathy is almost 9 times higher in diabetics than in the general population. According to scientific data, up to 50% of diabetics develop polyneuropathy. This makes diabetes the most common cause of polyneuropathy worldwide.
However, it obviously depends a lot on how severe the diabetes is and how it is treated. Those with only slightly elevated sugar levels obviously have a better chance of maintaining healthy nerves. In addition, diabetics who also suffer from vitamin deficiency, hypertension, dyslipidemia and obesity (severe overweight) have a greater risk of developing polyneuropathy, too.
If polyneuropathy does occur in diabetics, it is usually sensory polyneuropathy. That is, muscle strength is maintained while experiencing numbness, pain and discomfort or losing the ability to feel your feet or hands.
Things to consider in all types of polyneuropathies.
Regardless of the cause of polyneuropathy, there are things that should always be considered:
There should always be enough nutrients. In particular, vitamin D and vitamin B deficiencies may play a role in polyneuropathy. If there is a deficiency, it should be compensated. Normally, people consume enough of almost all important vitamins in a normal diet. Only vitamin D is very often deficient. According to the Robert Koch Institute, 56 per cent of Germans have less vitamin D in their blood than would be optimal(RKI).
However, this does not mean that you should flood your body with large amounts of vitamins. With all nutrients there is a certain optimal dosage. Taking more than that optimum does not add any benefit. It has often been tried to cure polyneuropathy by ingesting huge amounts of vitamins. These attempts have all failed. The body has a certain need for vitamins, as for other nutrients. If this need is covered, it is useless to take more. In the case of vitamin D, it is even dangerous to take too much. Usually, it makes sense to stick to the amounts indicated on the packages of vitamin preparations. A higher dosage should first be discussed with doctors or therapists.
For more on vitamins for polyneuropathy, click here:
Exercise can improve blood flow and processing of nerve signals!
In all forms of polyneuropathy, disturbances with blood circulation should be avoided. For better blood circulation, make sure you get plenty of exercise, especially endurance sports or special training for blood circulation. In addition, your diet should contain sufficient vitamin D and omega-3 fatty acids. Cholesterol should be kept within the healthy range as much as possible.
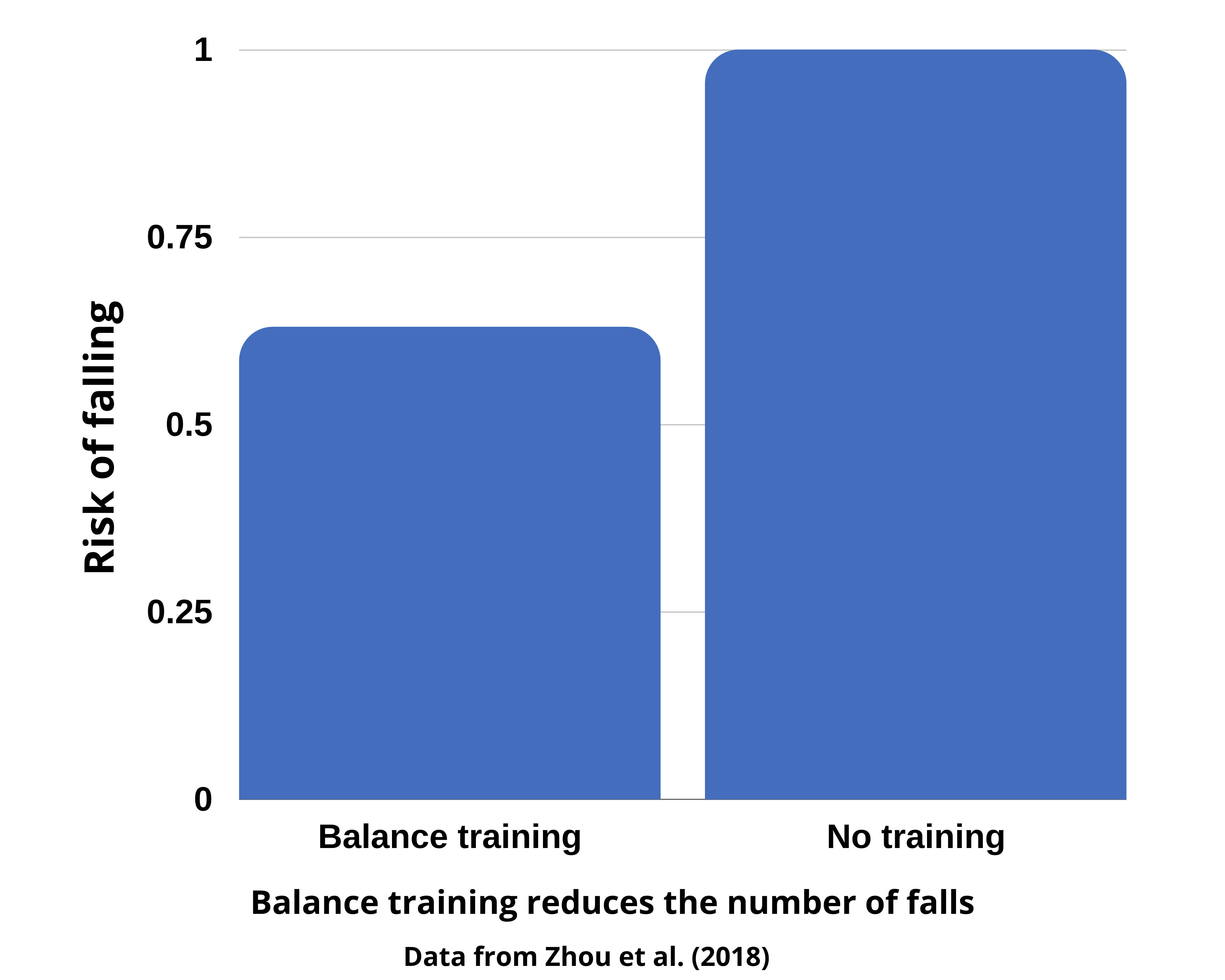
For all polyneuropathies, the quality of "signal processing" in the brain is also important. A well-trained nervous system is able to better process the signals coming from the damaged nerves and compensate for the damage to a certain extent. As a result, many patients experience less pain and better control over their movements. In particular, this leads to being able to walk more safely and stably, and to falling less frequently.
A detailed guide to exercises specifically for the nervous system can be found here: Exercise for polyneuropathy.
Why does polyneuropathy hurt?
The fact that polyneuropathy causes pain is somewhat paradoxical. Because actually, the main effect of nerve damage is that fewer signals reach the brain. This simply causes many patients to have less sensation in the feet and hands. However, other patients experience pain that can often be extremely severe. But why does it hurt to receive fewer nerve signals?
This is because of how the brain responds to polyneuropathy. The signals that the nerves transmit to the brain are received and processed there. When the signals become fewer and less conclusive due to polyneuropathy, the brain may adjust the "receiver" to be more sensitive. It's sort of trying to listen more closely and feel what's going on in the feet or hands. This can lead to even the smallest stimuli being perceived as pain. You could say that the brain overestimates the signals that are still arriving and considers the smallest signals to be a tremendous pain. A scientific paper on the subject can be found here: Domingues 2018
If you train the nervous system, especially by training balance and body awareness, then that seems to regulate this overreaction and thereby reduce the pain. While complete vanishing of the pain is rare even with balance exercise, however it is one of the few methods that can actually help and that you can easily do yourself at home.
You can find instructions on how to do this here: Exercise for polyneuropathy
You can find out more about pain in polyneuropathy here: Pain in polyneuropathy and what you can do about it
Muscle cramping contributes to the pain
In addition, pain often has more than one cause.
In my own patients, I very often see that in addition to polyneuropathy, muscle hardening develops, which also causes pain. Medically, this is called myofascial pain syndrome. I assume that the poorer perception of the body and the poorer control of the muscles contribute to the hardening.
It has already been shown with other painful conditions that a good perception of the body protects against the pain, because those who can perceive and control their body well are better at avoiding over- and incorrect loading of their bodies. On the other hand, those who can no longer perceive their body well due to polyneuropathy tend to adopt unfavorable movement patterns and bad posture. This also very often leads to overloading and hardening of the muscles.
Whether pain comes from muscles or nerves cannot be distinguished
In these cases it is not possible to distinguish whether pain is caused by nerve damage or muscle problems. The patient only feels "pain", it is not possible to distinguish whether this is caused by the damaged nerves or by the cramped muscles. Thus, the pain caused by cramped muscles should not be underestimated, although it is usually ignored in standard care of polyneuropathy. It is important to know that muscle problems can trigger pain in seemingly unconnected, far away locations. For example, toe pain is often triggered by the muscles that move the toes. However, these are located in the lower leg, such as the extensor hallucis longus, which is located on the shin and pulls the big toe up. When this muscle is hardened, you feel pain in the big toe, even though the hardened muscle is in the shin.
To treat such pain, there are several options:
1. massage the affected muscles to release the cramp.
2. stretching exercises to relax the muscles.
3. training your body awareness and muscle strength to prevent cramping and hardening.
See the following page for more information on how muscle stiffness makes the pain inpolyneuropathy worse and what you can do about it:
Diabetic polyneuropathy
Diabetic polyneuropathy is the most common form of polyneuropathy and affects somewhere between one-fifth and up to half of all diabetics. Diabetes causes several problems that can damage nerves and result in polyneuropathy:
Circulatory disorders
Deteriorated metabolism of nerve cells (especially mitochondria).
Accumulation of toxic waste products (so-called glycated proteins)
This gives you as a patient several starting points for the therapy: If you get the blood circulation and the metabolism going, then you also slow down the course of the polyneuropathy. The best way to do this is sports. Those who are well trained have a better metabolism and therefore lower sugar levels. Blood circulation is better in physically fit people. This also means that the toxic waste products produced by diabetes are removed more quickly and cannot damage the nerves. Therefore, it is essential for diabetics to exercise a lot and, above all, in the right way.
The training should include two main parts:
1. balance training to improve the function of the nervous system.
2. training sugar metabolism to lower blood sugar and improve blood circulation.
On the following page you will find detailed instructions on how to do this:
Sports and polyneuropathy
Sports play a significant role in polyneuropathy, especially to stay fit despite the disease. In some forms of polyneuropathy, exercise can also directly affect the disease. This especially is the case in diabetic polyneuropathy.
If you manage to reduce blood sugar levels through proper training, this will also positively affect polyneuropathy. It usually doesn't disappear completely, but at least it doesn't get worse as quickly.
In addition, sports and exercise can help maintain muscle strength, balance and flexibility. This can make it possible to walk better and not need a walker or a cane.
For detailed information, see these articles: Sport and polyneuropathy
Nutrition in diabetic polyneuropathy
Of course, diet also plays an important role in diabetic polyneuropathy. The fact that the sugar levels in your blood should be relatively low is of course obvious. Apart from this, you should make sure that the diet is good for blood circulation and inhibits inflammation.
Two important factors for this are vitamin D and omega-3 fatty acids. Both are good for the blood vessels and both are also anti-inflammatory. In addition, it is useful to eat only little red meat and not to smoke.
Severe obesity and elevated cholesterol should also be reduced as much as possible, as they also affect the blood vessels that supply the nerves.
You can find out more about nutrition in polyneuropathy here: Nutrition in polyneuropathy (in German)
Chemotherapy-induced polyneuropathy
Polyneuropathy due to chemotherapy is a problem that is starting to get more and more attention. With modern chemotherapies, some side effects are more controllable than with the agents used 20 years ago. However, polyneuropathies caused by chemotherapy are becoming more common.
This is because many of the different agents used in chemotherapy can also damage nerves polyneuropathies. You can find an overview of those in this table (not claiming completeness).
| Chemotherapy | Mechanismus | Besonderheiten |
| Platinum derivatives: Carboplatin Cisplatin Oxaliplatin | Damage of cell nuclei and mitochondria | Mostly sensory polyneuropathy Often further worsening after discontinuation (so-called coasting) With cisplatin, nerves to the head, e.g. auditory nerve, are often affected |
| Vinca-Alkaloids: Vincristin Vinblastin Vinorelbin Vindesin | Damage to microtubules | Mostly sensory polyneuropathy Often taste disorders Sometimes mononeuropathies develop (only one nerve is affected) Further aggravation after discontinuation may occur |
| Taxols: Paclitaxel Nab-paclitaxel Cabalitaxel | Damage to microtubules | Mostly sensory polyneuropathy Optic nerve damage can occur with cabalitaxel |
| Proteasome Inhibitors: Bortezomib Carfilzomib Ixazomib | Not known exactly | Often small fiber polyneuropathy |
| Angiogenesis inhibitors: Thalidomid Lenalidomid Pomalidomid | Disturbance of blood circulation | Frequent disruption perioral nerves (surrounding the mouth) |
Exercise seems to protect nerves during chemotherapy
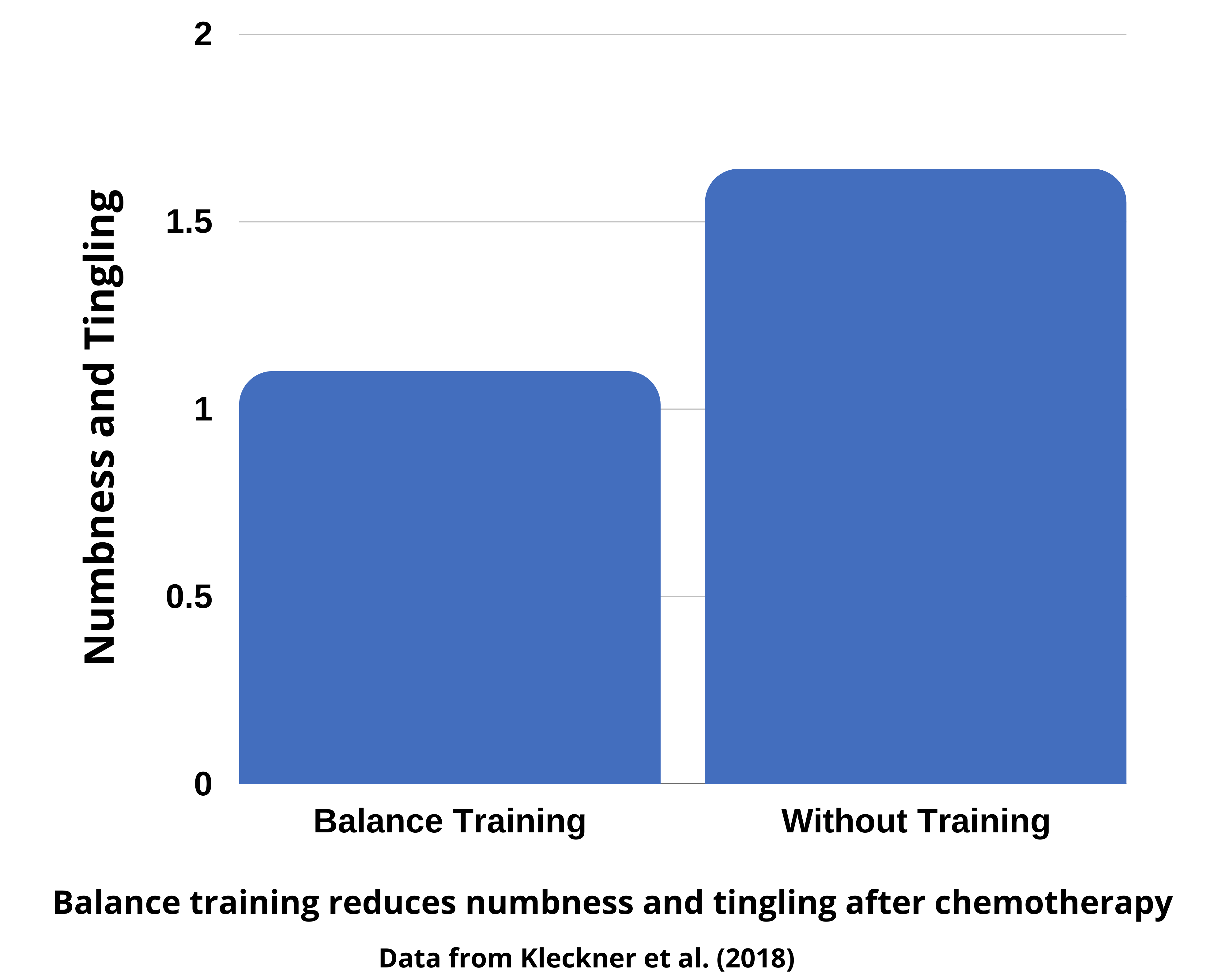
Continuing to exercise during cancer treatment has numerous positive effects and may even improve chances of survival. For polyneuropathy, balance exercises have proven to be specifically effective. Exercise during chemotherapy reduced symptoms of polyneuropathy in a study of lymphoma patients (Kleckner et al. 2017). However, this only seems to work when actual balance exercises are performed. Pure strength and endurance training has comparatively small positive effects on polyneuropathy.
In a study at the University of Freiburg, it was observed that patients who particularly trained their balance recovered more quickly after chemotherapy. During the study period, 87% of patients who exercised reported improvement, while no one (!) in the inactive control group felt improvement(Streckmann 2014).
A detailed guide to exercise for polyneuropathy can be found here:
Exercise for polyneuropathy
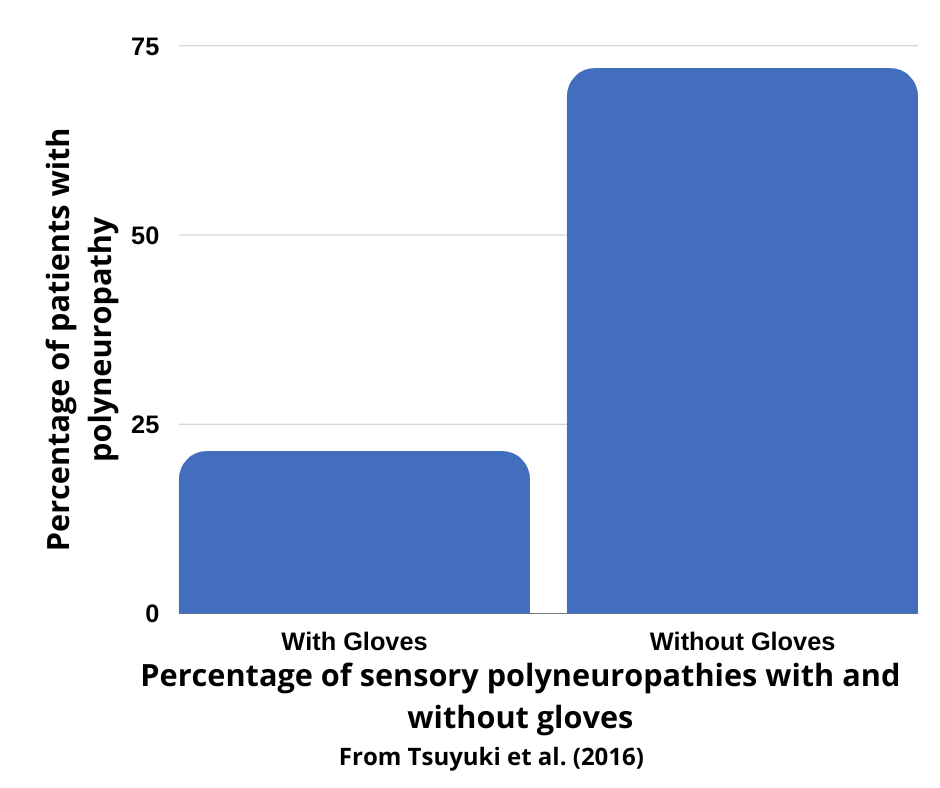
Prevent polyneuropathy with gloves
However, in addition to exercise, it is also useful to protect the nerves during the administration of chemotherapy. This is done by putting on tight gloves or compression socks that compress the hands and feet. As a result, less blood flows to these parts of the body and thus less chemotherapy agent reaches them, which could damage the nerves.
This procedure is very simple, low risk and cheap. You can get gloves for just a few cents each. It is important that the gloves are tight enough. Therefore, you should use gloves that are one size smaller than your actual size. You should also put on two gloves on top of each other to achieve the necessary compression.
For the feet you can use compression socks. These are now available not only as models for medical purposes, but also for athletes, which are more comfortable to wear.
Let's get this right: normally good blood flow is a prerequisite for good health, only during the short period of time when the active ingredients of chemotherapy are in your blood it makes sense to decrease blood flow in certain parts of your body. Therefore, it is also only useful to wear gloves and compression stockings during this short period of time.
Results of wearing gloves
In a Japanese study, wearing the gloves produced impressive effects. During the administration of paclitaxel, patients wore the gloves as described, but only on one hand. The other hand was not treated.
Patients were much less likely to develop polyneuropathy on the hand protected by the gloves, while the other hand very frequently showed symptoms of polyneuropathy.
You can read the study here: Tsuyuki et al. (2016)
Incidentally, in another study it was shown that a similar effect can be achieved by cold when compression is not possible (Kanbayashi 2020).
Protection by omega-3 fatty acids
Besides exercise, of course, nutrition also plays an important role in chemotherapy.
So far, omega-3 fatty acids have also proven their worth here. With both paclitaxel and bortezomib, nerves appear to be protected by omega-3 fatty acids (Maschio et al. 2018; Anoushirvani et al. 2018)
However, it seems crucial to consume omega-3 fatty acids from the ocean. Plant-based omega-3 fatty acids don't seem to work. The good news here is that there are preparations with fish or algae oil for little money in most drugstores. However, it is recommended to talk to your doctor about such supplements instead of simply taking a supplement on your own.
For more tips on nutrition in polyneuropathy, click here: Nutrition for polyneuropathy (in German)
In some cases, acetyl L-carnitine helps (probably).
In some studies, positive effects of acetyl-L-carnitine were observed in polyneuropathy due to chemotherapy. However, this is only the case with certain chemotherapies and does not generally apply to all chemotherapies that can cause polyneuropathy.
Apparently, an effect can only be expected with platinum derivatives (e.g., cisplatin, carboplatin, oxaliplatin). Other types of chemotherapy (e.g., taxanes) showed no effect in the available studies.
A scientific review on this can be found here: Dinicola et al. 2018.
However, be sure to talk to your doctor before taking supplements during chemotherapy, as it cannot be ruled out that they may interact with chemotherapy or other medications or reduce the effectiveness of chemotherapy.
Alcoholic polyneuropathy
Alcoholic neuropathy is one of the lesser known consequences of alcoholism, but it is very common. Depending on the severity and duration of the alcoholism, between one-fifth and one-half of alcoholics are affected. Women appear to be somewhat more susceptible to the nerve damage caused by alcohol than men.
Alcohol harms on several levels at once:
Alcohol is toxic and can directly damage nerve cells.
Alcohol depletes B vitamins, which are important for nerve function and without which polyneuropathy can develop.
Alcohol worsens blood circulation in the long term (Puddey et al. 2001) and therefore the supply of the nerves.
Alcohol increases inflammation(Alcohol and Inflammation).
It could play a role in which alcoholic beverages one consumes. Beer, for example, contains B vitamins that could somewhat offset the effect of alcohol. Red wine may be slightly less damaging to circulation than other beverages because of the polynphenols it contains. Alcohol in the form of liquor or vodka, on the other hand, is probably more dangerous.
Alcohol, by the way, can not only damage the peripheral nervous system, but also cause damage directly to the brain. This can lead to alcoholic dementia.
Even people who are not commonly thought of as alcoholics can develop polyneuropathy from alcohol consumption. For example, someone who drinks three pints a day is not generally considered a drunk, yet this can already contribute to nerve damage. This is particularly the case when several risk factors come together. For example, anyone who suffers from diabetes and also drinks regularly increases his or her risk.
Incidentally, a significant role in the development of nerve damage is played by the frequency of drinking. Those who rarely drink heavily do less damage to their nerves than those who drink daily(Chopra & Tiwari 2012).
You have to keep in mind that the dosage is crucial. The famous one glass of red wine remains healthy as long as it actually stays ONE glass.
Polyneuropathy of unknown cause
Very many patients tell me: I do not have diabetes, never had chemotherapy and do not drink alcohol, yet I suffer from polyneuropathy.
This is a very unsatisfactory situation, because of course one would like to know what is the cause of the polyneuropathy. Unfortunately, however, this happens very very often. One reason is that polyneuropathy is a disease that often has more than one cause. An unfavorable predisposition, an unnoticed vitamin deficiency and a circulatory disorder, for example, can go hand in hand and together cause polyneuropathy. In such cases, it is simply not possible to determine exactly which factor triggered the polyneuropathy.
If the cause of your polyneuropathy is not known, however, then you should be careful to take as many measures as possible to protect the nerves:
- Train your balance to maintain good body awareness
- Ensure good blood circulation through physical exercise and good nutrition
- Make sure you get enough vitamins, especially vitamin D and B vitamins
- Stretch and massage your muscles to reduce hardening and cramping.